Natural Implant Restoration in Stable Alveolar Bone(NIRISAB)—Concepts in Clinical Practice


Link to This Clinical Case Report
Click here to download the report.
Author: Dr. William Liang, DMD
One of the most challenging aspects of dental alveolar ridge augmentation surgery is achieving proper wound closure and uneventful healing. To date, most of the open flap approaches have been fraught with complications. Many of these complications can be eliminated if the soft tissue incision is placed away from the surgical site. This paper describes the clinical application of a remote incision in various ridge augmentation surgeries as developed by Dr Hilt Tatum. It is part of the concept of natural implant restoration in stable alveolar bone that Dr Tatum introduced in the early 1970s.
Introduction
Currently, a common approach to bone grafting is guided by the adage of surgery that one must be able to physically see the surgical site. It is logical, based on the premise, that surgical access be prefaced by proper flap design and reflection. It is equally reasonable that these access flaps be coapted in a tension-free, primary closure manner.1 This approach, although it follows sound surgical principles, is fraught with complications and compromises.2–5 Incision line failure (opening) is observed in upward of 20% of guided bone regeneration procedures.6
Postsurgical incision line failures occur for various reasons. The incision and reflection process damages the soft tissue integrity. The damaged soft tissue then must reattach to the bone; however, the biological time-dependent process of wound healing dictates a period of vulnerability to the site. Tissue integrity is compromised because of surgical trauma and may be further compromised if there is tension within the flap. Bacterial ingress and/or physical trauma at the incision region is always a threat. The latter can be from food impaction, muscle pull, and pressure from adjacent structures such as the tongue, and even normal function such as deglutition or speech may interfere with the timely healing of the incision site.4 The act of suturing and the frequency of punctures to the tissue as part of suture placement process also compromises the blood supply and tissue integrity at the incision line. The act of releasing the
periosteum compromises the blood supply of the overlying soft tissue and further increases the risk of incision line failure. Finally, suturing the soft tissue flaps over a nonvital graft material devoid of blood supply is never ideal for healing. Therefore, surgical success may be greatly enhanced if incisions are avoided over graft material.
As early as 1967, James Alley demonstrated the remote incision and tunnel approach to bone grafting on denture patients. In 1970, Hilt Tatum used the technique for bone grafting and subsequent implant placement.
The remote incision and tunnel approach to bone grafting are 2 fundamentally game changing principles that bears examination. The concepts are part of a larger philosophy of natural implant restoration in stable alveolar bone (NIRISAB) that was developed in the 1970s and first presented by Hilt Tatum at the 2004 AAID annual conference. Although it was generously taught at some AAID Maxicourses by Dr Tatum since the 2000s, it was not widely published. More recently, the tunnel approach to ridge reconstruction received favorable reports,7–11 but the concept of remote incision was not mentioned or emphasized in many of the techniques described.
The relocation or repositioning of the access incision away from the surgical site avoids the potential of incision line failure directly superficial to the graft material. The working access is achieved by tunneling from the incision placed at least 1 tooth anterior to the recipient site. The raised tunnel, with the periosteum intact, provides a means of containment of the graft material. The technique allows the surgeon to mold and shape the graft to the ideal desired contour. The tissue tension naturally assists in form maintenance of the graft during healing. Soft tissue failure over the graft rarely occurs. If the incision line opens, it does not affect the graft because it is at a location remote to the graft site. This article presents 3 clinical cases with 10þ-year follow-up results of 3 bone grafting modalities (case 1, tunnel particulate graft; case 2, tunnel allo-block graft; case 3, Tatum vascularized osteotomy). All 3 modalities used the philosophy of NIRISAB. Of particular emphasis in this article is (1) the surgical approach of tunneling, (2) lack of a crestal incision, and (3) a remotely placed access incision.
AAID Vancouver MaxiCourse, University of British Columbia Continuing
Dental Education, Surrey, British Columbia, Canada.
Corresponding author, e-mail: wliang@implant.ca
https://doi.org/10.1563/aaid-joi-D-22-00032
Case 1: Bilateral Tunnel Particulate Grafts of Div C-Wh Single Tooth Edentulous Sites
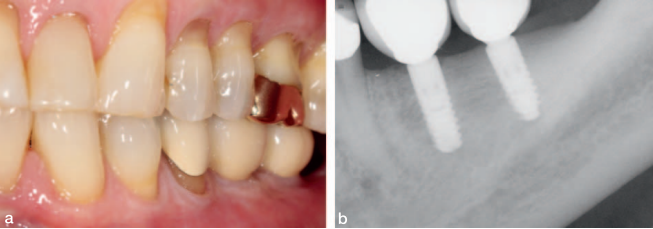
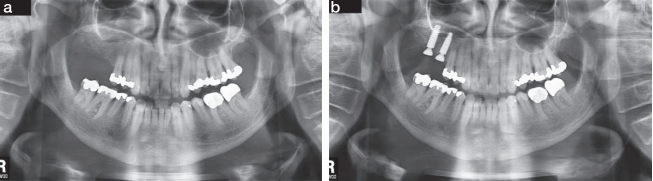
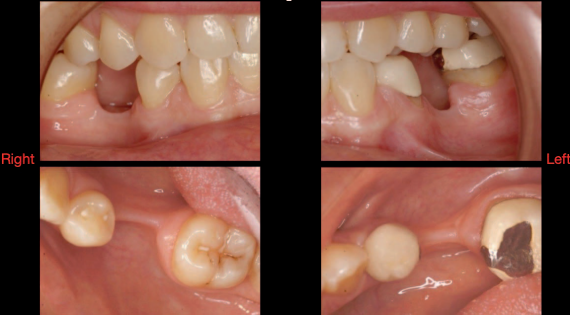
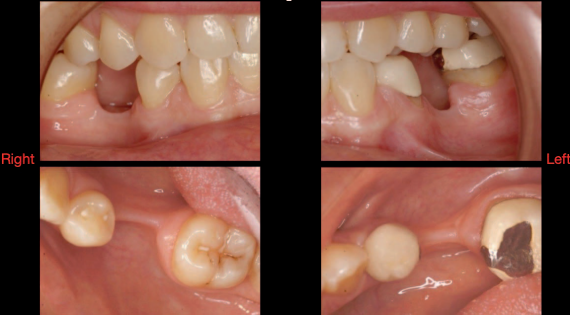
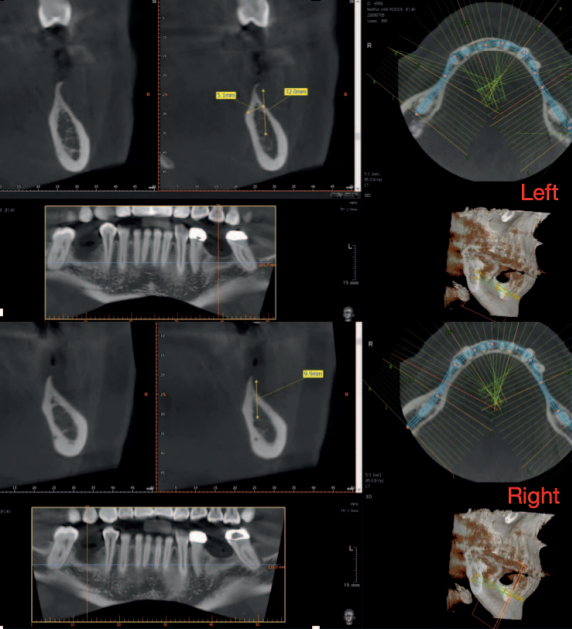
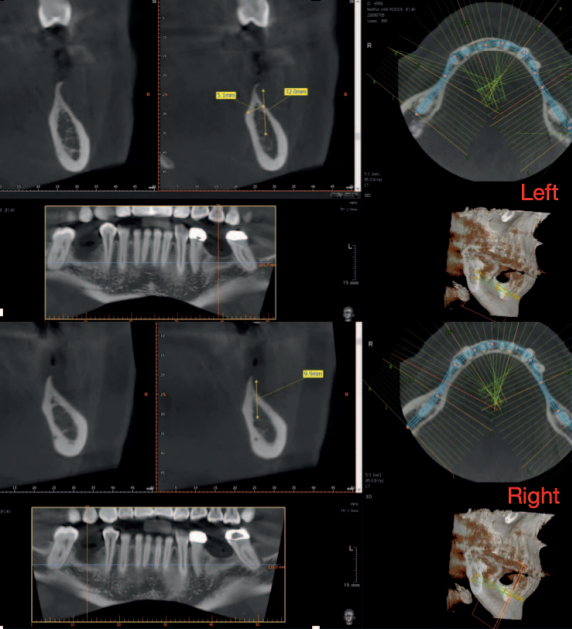
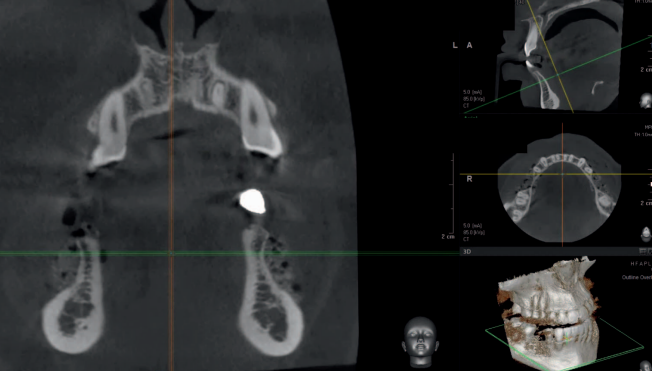
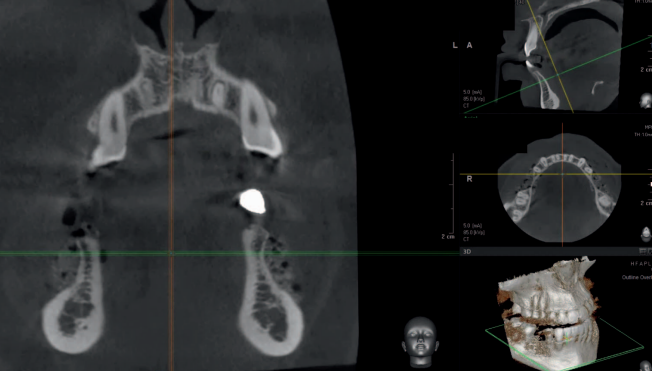
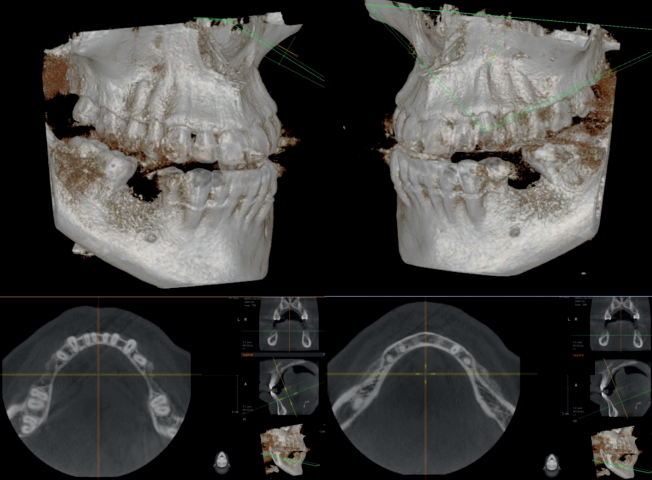
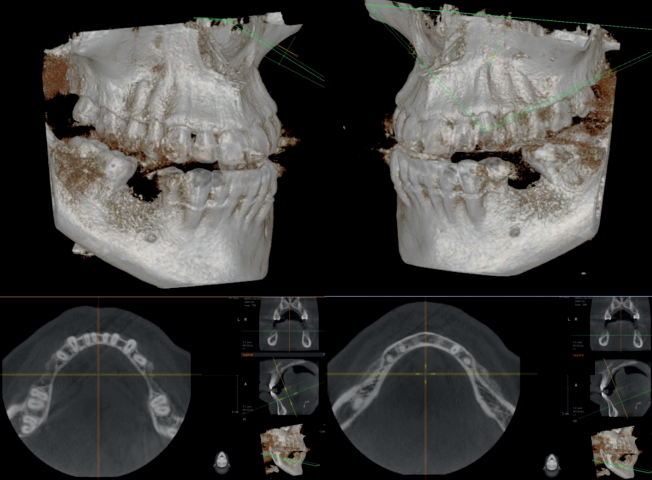
In August 2009, this 42-year-old female patient (ASA I) presented to the clinic with Applegate-Kennedy CL3 bilaterally missing lower first molars. The residual ridges were Div C-wh.12 The patient was previously told that dental implant treatment was not possible because of the lack of bone at the sites. Furthermore, she was told that it was not possible to rebuild the lost bone.
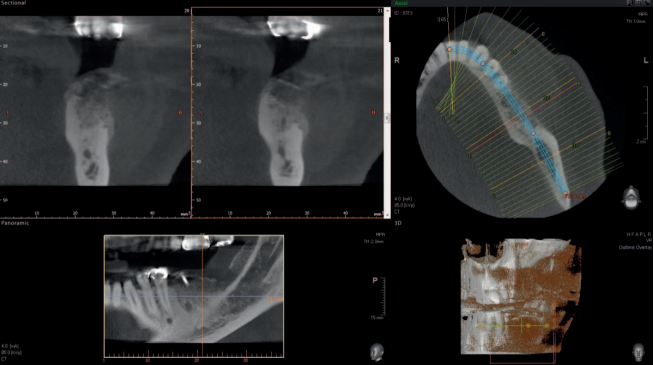
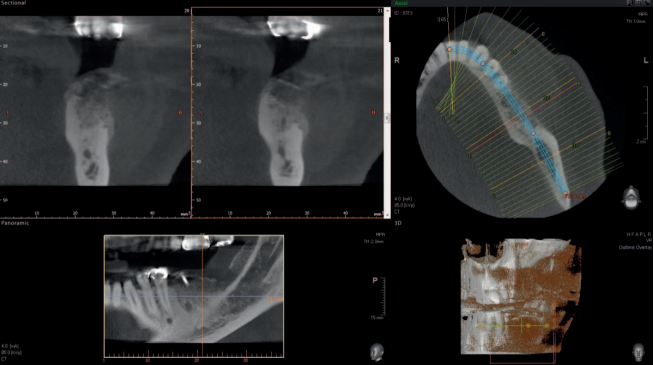
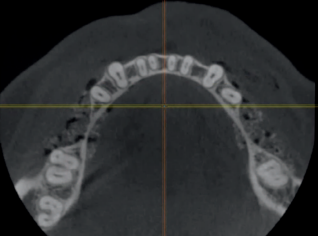
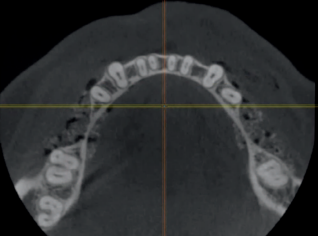
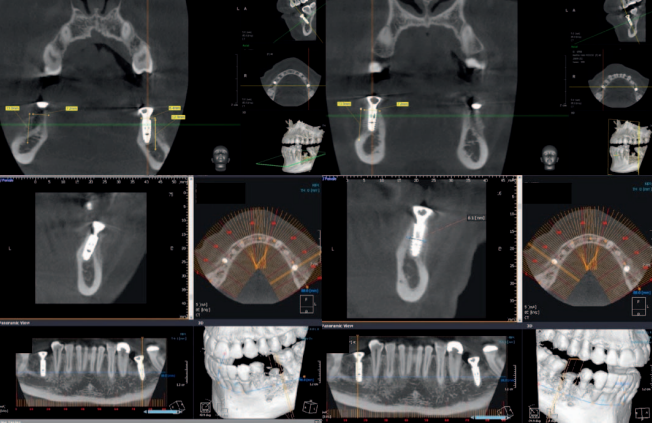
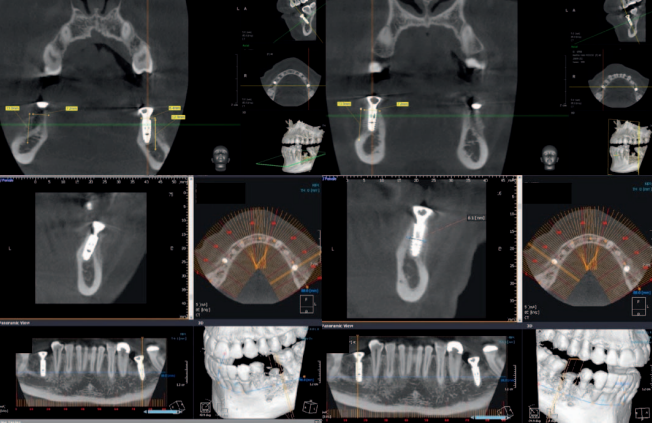
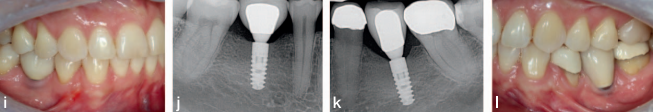
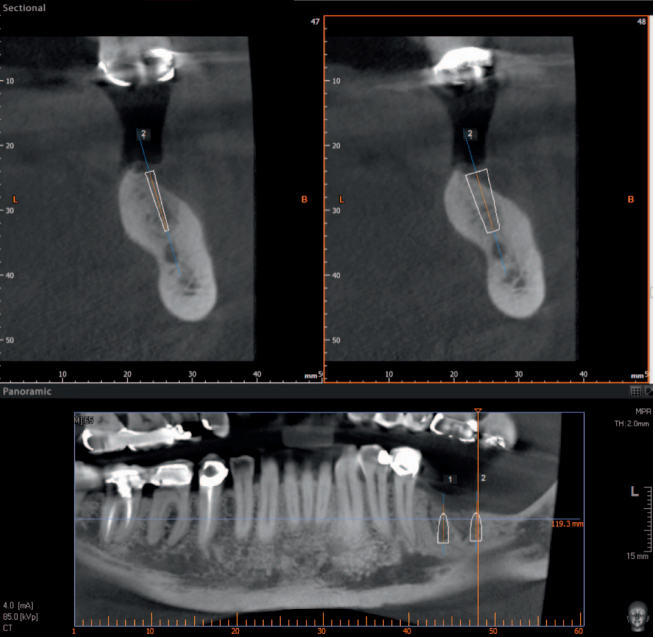
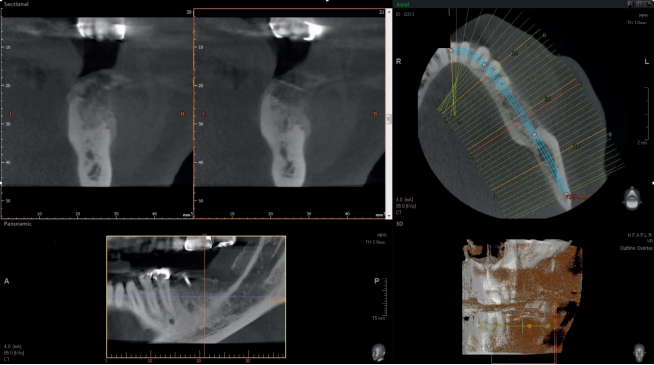
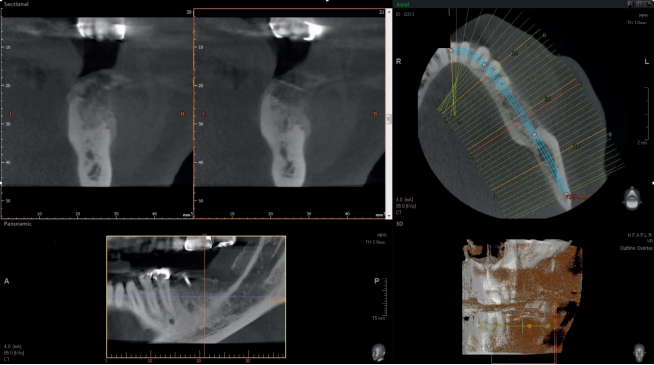
The edentulous sites had been missing the second premolars and first molars for an unknown time. The edentulous spaces, however, had been reduced to the dimensions for single molars through mesial drifting of the posterior teeth. Although the diagnostic CBCT images showed that the residual ridges may be modified to accommodate division B implants (3.0–3.5 mm diameter), the resultant crown :implant ratio of 2:1 would be bio-mechanically unfavorable. If the deficient ridge was left uncorrected, food impaction could be a potential complaint from the patient. Of less importance is the esthetic compromise of the final prosthesis. Therefore, ridge reconstruction was recommended using a particulate graft to regain ridge width. The patient was informed that any gain in ridge height would be a bonus, but the main goal was to regain an adequate amount of ridge width for implant placement and ultimately improve on the implant position (Figures 1 and 2).
Material and methods
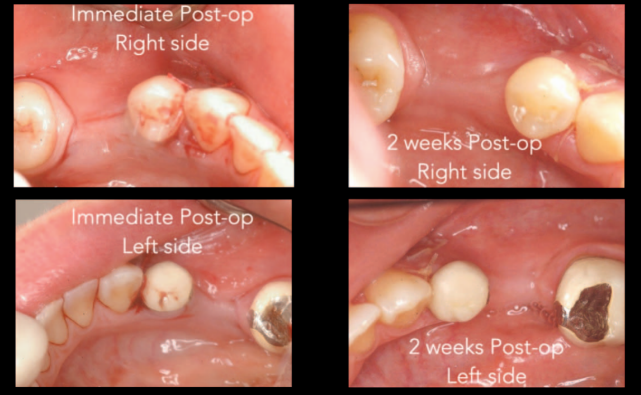
Both sites were treated using identical techniques and material. A tunnel approach particulate bone graft was performed using a remote anterior incision that placed 1 tooth anterior to the edentulous graft recipient site. The flap was reflected using a Molt 2/4 elevator and a Prichard elevator to achieve a relaxed soft tissue tunnel exposing the residual bony ridge. The tunnel was extended lingually slightly beyond the lingual mucogingival junction. Decortication of the buccal cortical plate was achieved using a #4 straight surgical round bur to encourage the regional acceleratory phenomenon (RAP). A Bioguide porcine collagen membrane (Geistlich Pharma North America, Princeton, NJ) was inserted to support the roof of the soft tissue tunnel. A bone mixture of approximately 1 mL of Rocky Mountain cancellous bone and PRP plus clindamycin was placed from the anterior access point into the tunnel (Figures 3 and 4). Once sufficient bulk was achieved, the site was checked for passive flap closure by placing the cut edges to lie passively along each other. The incision line was sutured closed with 4/0 Vicryl sutures (Ethicon, Cincinnati, Ohio) using a combination of sling and continuous interlocking techniques. Postoperative medications consisted of ibuprofen 600-mg tablets for analgesia as needed, a mild tapering dose of decadron for 3 days (4, 2 and 1 mg), and a course of antibiotics of clindamycin 300 mg, 3 times per day, for 1 week. Figures 5 through 7 highlight the postoperative appearance of the graft material in situ, whereas Figure 8 illustrates a comparison of the preoperative and postoperative appearance of the ridges.
Postoperative home care was to resume as usual with light brushing around the surgical site for 1 week and suture removal in 2 weeks. The patient was instructed to avoid chewing of any kind at the back of her mouth.
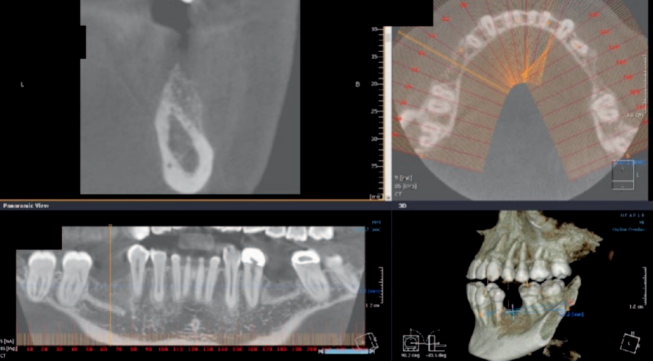
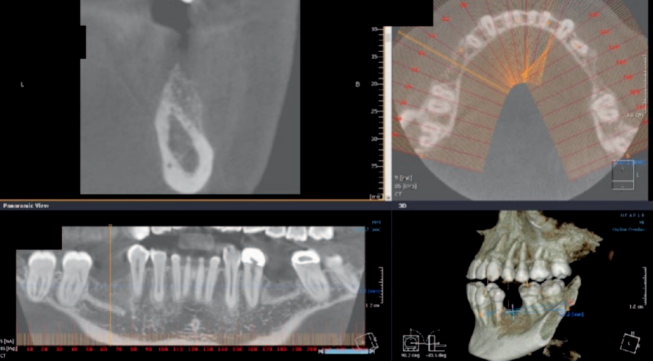
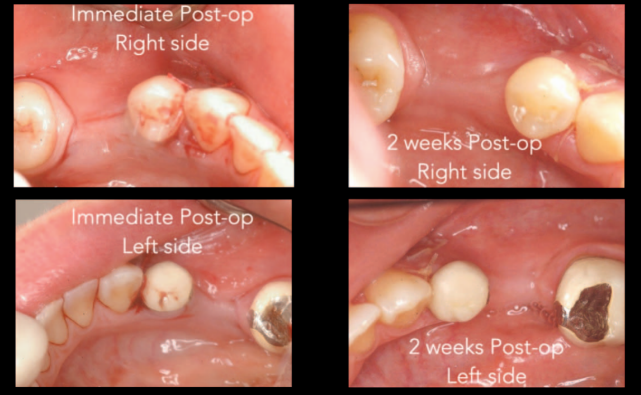
Sufficient bulk was achieved for both the deficient residual ridges, and the sites healed uneventfully. Div A-h ridges were achieved bilaterally after 4 months of healing (Figure 9). At that point, Ankylos A 9.5 mm- x 3.5 mm-diameter implants were placed with a single-stage approach for the sites. Because the sites, being edentulous for some time, were lacking in the amount of keratinized gingiva, they were minimally reflected for implant placement. The buccal contour deficiency and the lack of keratinized tissue were corrected at the time of implant placement using the vascularized buccal inversion flap (VBIF) technique described by Liang.13


After 4 months of healing, the site exhibited significant bone formation with a density of D4 for the de novo bone. A new buccal cortical plate was visible at the outer expanse of the lower CBCT scan (Figure 10). With the newfound bony ridge being Div A, implants were able to be placed in the correct position with a Cr/I ratio of 1 or less. Implant placement was uneventful other than minor disturbances to the newly formed bone.
One of the principles of NIRISAB is to avoid flap exposure of the bony ridge on reentry for implant insertion. On the right side, the buccal flap was reflected slightly more aggressively than the left side. As a result, a portion of the crestal grafted bone on the right side separated from the newly formed ridge and was repositioned back in place, secured by the flap and a sulcus former (Figures 11 and 12)
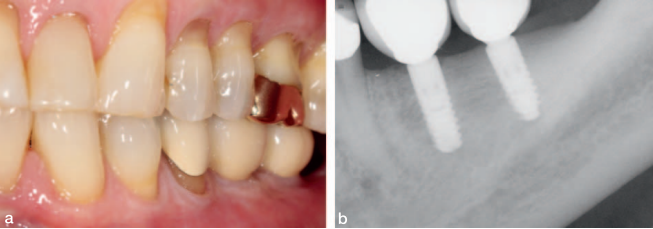
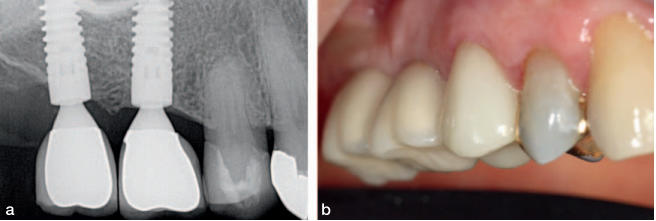
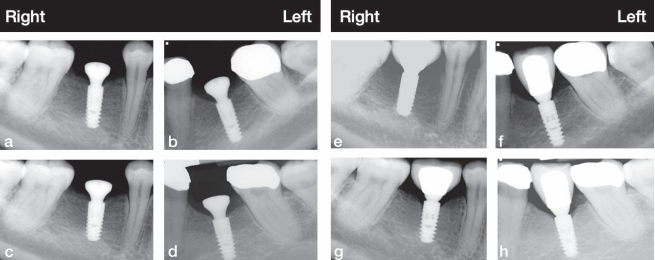
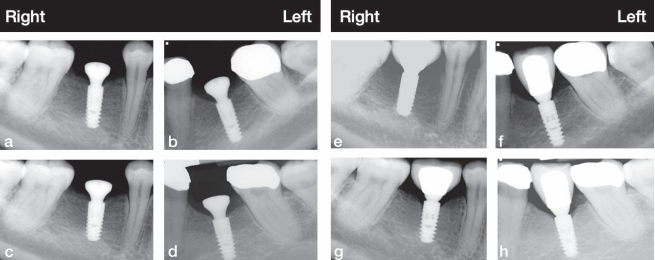
The crestal bone level was well maintained over the initial integrating period. Subsequent radiographs taken at 1, 3, and 12 years demonstrated that the crestal bone level was unchanged and possibly improved (Figures 13 and 14).
Because most of the implant body is positioned in the grafted bone, its stability is of vital importance for maintaining the implant’s function.
Results
This case has been stable for 12 years. The result demonstrates that the tunnel particulate graft approach to ridge reconstruction using a remote incision is a viable modality for ridge reconstruction in single tooth sites.
Case 2: Tunnel Allo-Block Graft
This case was treated in 2012. A healthy ASA II 65-year-old man presented with an Applegate-Kennedy Cl 2 edentulous site in quadrant 3. He was missing the lower left first, second, and third molars. His remaining dentition was periodontally stable and well restored. The residual ridge was Div C-hw.
A common approach to treatment would involve accepting the height deficiency of the residual ridge and to restore the area using short implants. Attempts to improve the ridge dimensions often focus on regaining ridge width and not height. This is based on the abovementioned notion that incision line opening is a common complication of grafting for vertical ridge height. A tunnel approach to accommodate a bone block would circumvent this potential complication. In this case, a tunnel allo-block graft was the chosen reconstruction modality to regain ridge width and height.8,10,14–16
Materials and methods
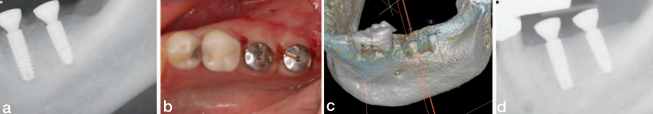
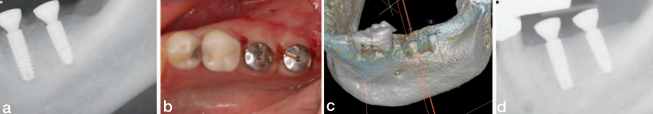
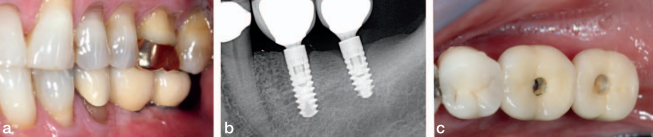
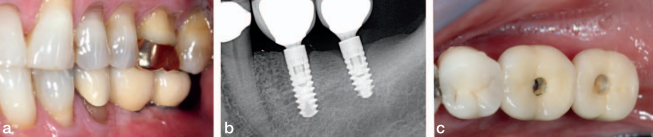
Like case 1, a remote access incision and tunnel approach were established 2 teeth anterior to the edentulous site. An allograft block from vertebral bone was used (Rocky Mountain Tissue Bank, Aurora, CO). After sufficient access was achieved from the elevation through the tunnel, an ACE surgical 20-mm x 30-mm type 1 collagen membrane was trimmed to fit the site. A single 10-mm surgical screw was placed vertically, 5 to 10 mm distal to the second premolar from the anterior access of the tunnel to stabilize the graft. It was determined that the graft was stable against the residual ridge, and a second screw was not necessary. In addition to suturing with 4/0 PTFE sutures, the wound was dressed with periodontal dressing (Coe PaK, Coe Laboratories, Alsip, Ill). The site was left to heal for 4 to 6 months (see below for explanation). During that time, some of the allograft became exposed at 4 months (Figure 18a). The exposed bone was removed, and the site was decontaminated regularly by the patient with daily application of chlorhexadine gluconate 0.12% rinse (Colgate Oral Pharmaceuticals, Lakewood, NJ). The dehiscence healed naturally afterwards at 6 months (Figure 18b). The resultant gain in bone height varied from 6 to 9 mm (Figures 18c and 19).


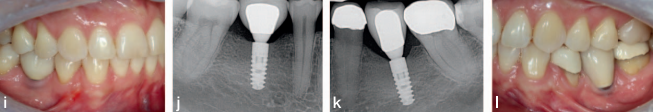
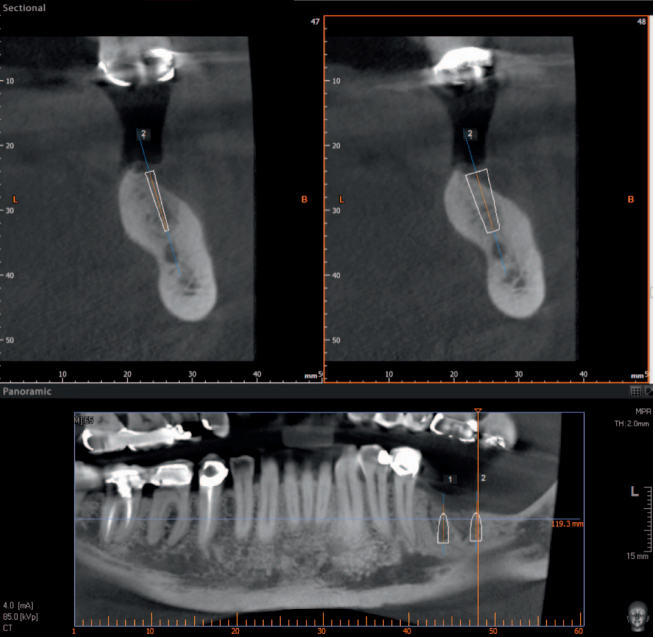
After 6 months, the native de novo bone had Ankylos A14 (in position #19) and A11 (in position #18) implants placed using a single-stage approach. The soft tissue was closed using the (VBIF) (Figure 20).
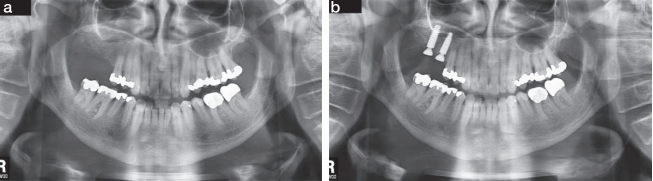
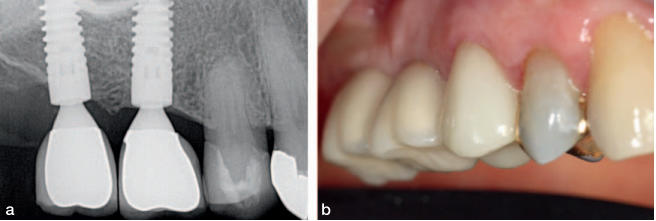
The final screw retained restoration is documented in Figure 21 showing a healthy radiographic crestal bone level. The same views of the restorations at 2 years in Figure 22 shows a stable restoration in function. The patient returned to his general dentist for routine maintenance after year 2. At year 10, the patient was examined at our clinic. He reported no clinical symptoms and offered that he has not had any need to think about his implants. He had been completely comfortable for the last 10 years. There was evidence of neglect because the occlusal seals of the implants’ supported crowns were missing, and food was impacted in the screw access (Figure 23c). Radiographic bone loss was also evident (Figure 23b). Gingival health, however, appeared normal (Figure 23a), as the periimplant tissue displayed normal color, texture, and tone. The peri-implant readings were all less than 3 mm on probing.
Results
This case demonstrated that a resorbed ridge deficient in height may be regained using a structured bone block. In this case, an allograft block was used. One of the challenges for lower posterior edentulous sites is that the overlying soft tissue is often thin and devoid of keratinized gingiva and/or connective tissue. An allograft in a block form is more rigid than particulate graft material and therefore more likely to perforate the overlying mucosa tissue. A tunnel approach for this type of graft may be able to delay the perforation and allows the bone block to revitalize in vivo. A late-stage exposure of the graft is easier to manage as the graft will be vascularized at the time of exposure. Despite good surgical intervention, the long-term outcome for any case largely depends on ongoing maintenance and home care. In this case, lengthy neglect by the patient, perhaps because of overconfidence of the results, led to some compromises. Intervention at this stage will include assessment for parafunction, occlusal interference, peri-implant hygiene, and patient oral health care to alleviate or remedy the peri-implant pathology and prolong the life of the implants. The fact that the grafted bone has withstood the biological and perhaps mechanical insult because of neglect is a testament to the success of the original
reconstruction.
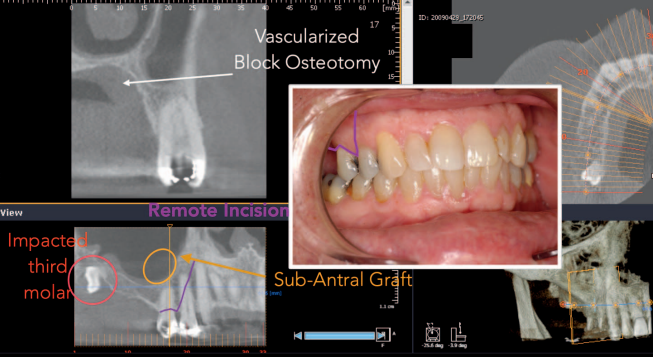
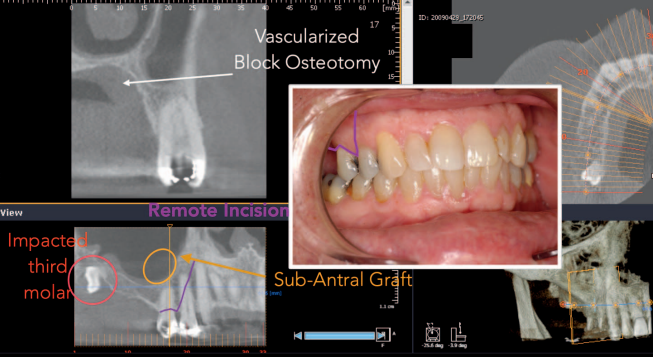
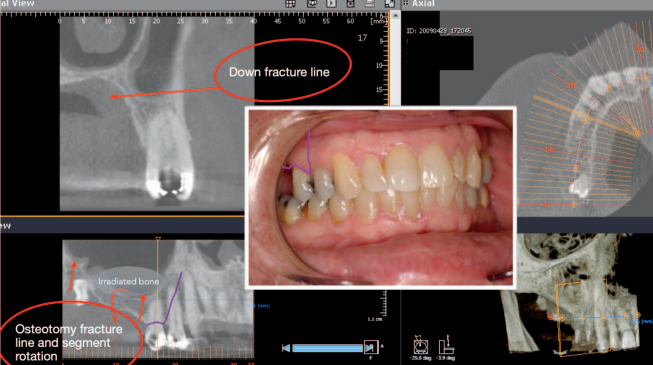
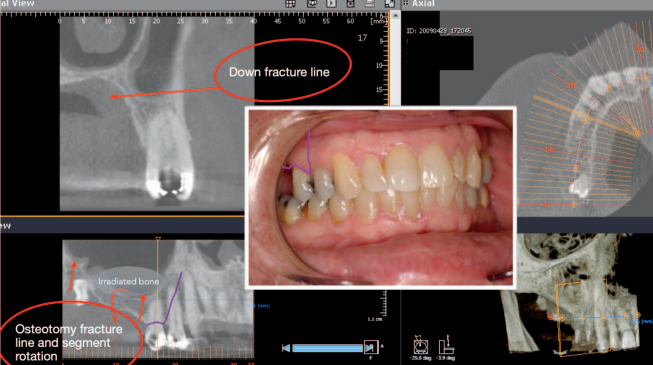
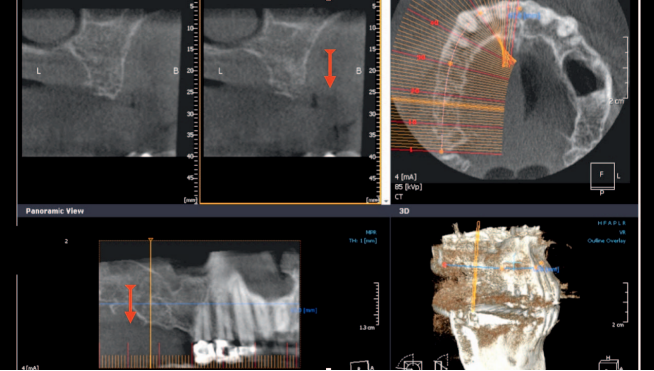
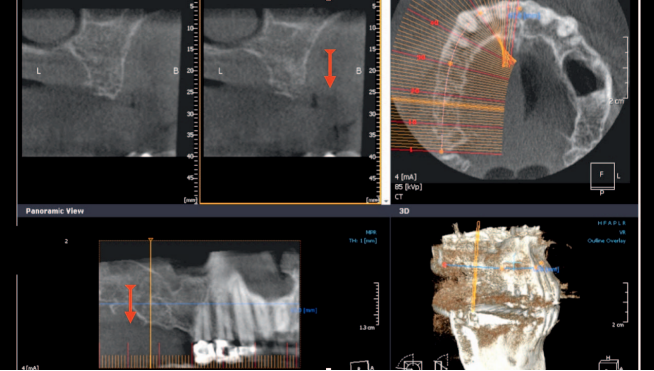
Case 3: Tatum Vascularized Osteotomy With SA4 Subantral Augmentation
This patient was an ASA II 65-year-old man at the time of treatment in 2009. He displayed a maxillary right Applegate Kennedy Cl 2 edentulism, missing the upper right first and second molar. The upper right third molar was impacted. The residual ridge was Div C-wh. A treatment plan consisting only of subantral augmentation and implant placement with the existing crestal height loss (Figure 24) would compromise the outcome and disregard the principles of NIRISAB. The ideal outcome would involve the restoration of posterior ridge height. The prescribed treatment plan involved the removal of the impacted upper right third molar in conjunction with a subantral augmentation and a tatum vascularized osteotomy (TVO).
noticeable.
Materials and methods
A remote incision flap was elevated 1 tooth mesial to the edentulous site. Similarly, a flap was raised from the tuberosity to the distal vestibule to allow access for the removal of the impacted upper right third molar. A vascularize osteotomy was performed where the periosteum over the mobilized bone block remains attached to the segment. A Rocky Mountain Tissue Bank allograft bone block was interposed between the floor of the sinus and the mobilized ridge to reposition the crest of the ridge coronally. Cancellous bone from the Rocky Mountain Tissue Bank was placed in the subantral space. Primary, tension-free closure was achieved using Vicryl 4/0 sutures (Ethicon) (Figures 24 through 27).
After a 4-month period of healing, a Div A ridge was achieved. Two Ankylos A 14 (3.5-mm-diameter x 14-mm-length) implants were placed using a single stage approach (Figure 28). The implants were restored with cement retained crowns after an integration period of another 4 months (Figure 29). With proper occlusal management, regular intervals of professional supervision, and proper home oral hygiene, the 7- and 12-year radiographic and clinical examinations demonstrate largely unchanged crestal bone level and stable periimplant soft tissue.
Results
Although this was not intended to be instructional for the management of posterior bone height loss in the maxilla, it does highlight the possibility of using a tunnel approach and remote incision to regain the lost alveolar ridge. The significance of remote incision combined with a tunnel approach are paramount in the avoidance of graft exposure regardless of the type of graft material used. In these complex cases, graft exposure may result in serious consequences and severely compromises the clinical outcome.2–4
Discussion
The end goal of NIRISAB is to achieve a natural looking and functioning implant supporting restoration in stable alveolar bone. It implies that the alveolar bone must be restored to its
former dimensions, and its restored dimensions must be sustainable even in function. These 3 case presentations highlight 2 of the core principles of NIRISAB. They serve several common purposes.
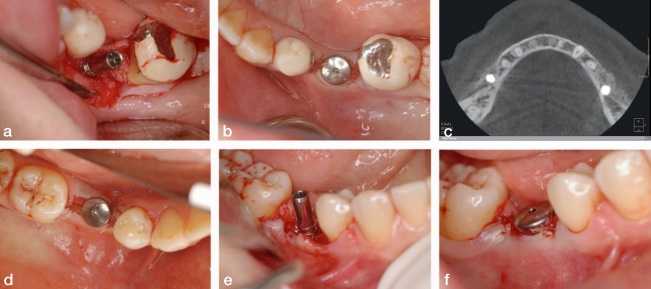
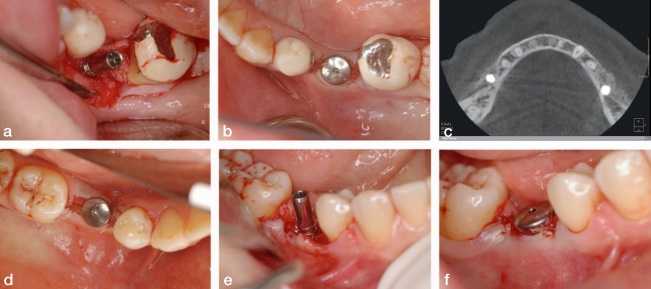
disturbed at the time of implant placement. (f) Sutured implant site using the VBIF technique.
The first is to maintain vascular integrity to protect and supply nutrient to the graft recipient site. Tunneling avoids severing of the vascular anastomosis at the edentulous crest, whereas a remote access incision moves the compromise away from the graft site. If an incision is used at the edentulous crest, the flap will be weakest at that area and be reliant on sutures to maintain closure. Any pressure from function or edema will invariably be concentrated at, and potentially breach, the incision line. Often, clinicians will score the periosteum to release the dense fibers to achieve a passive flap. This action further compromises the integrity of the flap and may in fact contribute to postoperative pain and incision line failure. The undisturbed blood supply in the tunnel design allows for vascularization of the graft immediately after placement, which should provide a significant advantage compared with the open approach.
Second, the volume of the graft material will stress and distend the overlying soft tissue. The advantage of the tunnel approach is the even distribution of the tension on the overlying tissue. Aside from the lack of stress concentration because of a non-existent incision line, the overall tension on the flap assists in containing the graft material at its desired position.
The third advantage of this approach by its inherent design is the ability to mitigate damage in the event of an incision line failure or a perforation of the overlying soft tissue above the graft. If the anterior access incision fails, it is at least a tooth or approximately 8 to 10 mm away from the graft material, which minimizes the contamination of the graft. Healing by secondary intention is most often achieved without incident. Perforations of the overlying soft tissues, when it does occur, usually involves block grafts. These perforations with block grafts tend to occur later in the healing process. Such delayed soft tissue failures are more correctable because the graft has had some time to vascularize, and the risks of total graft failure are reduced compared with an incision line failure within a few days after a crestal incision graft approach. More modern approaches using various biologics and adjuncts such as platelet-rich fibrins to insulate the block grafts under the soft tissue tunnels have provided anecdotal improvements in outcomes.




The application of the NIRISAB philosophy requires a modified approach to surgical design. It encompasses concepts and design principles for surgical access and techniques for surgical manipulation of bone. This complex topic is beyond the scope of this paper. It is evident, however, that the benefits of remote incision and closed flap approach is universal regardless of the graft material or biologic adjuncts used. It is not a novel technique because it has been in use since the 1970s, but it is one that should be used more frequently. This approach is perhaps less popular because it is more difficult to achieve. Access to the surgical site is limited and often requires careful circumvention of vital structures. Additional quantitative and larger-scale comparative studies will most likely further validate this surgical approach.
Note
The author declares no conflicts of interest.
References
- Wang HL. ‘‘Pass’’ principles for predictable bone regeneration. Implant Dent. 2006;15:8–15.
- Fugazzotto PA. Maintenance of soft tissue closure following guided bone regeneration: technical considerations and report of 723 Cases. J Periodontol (1970). 1999;70:1085–1097.
- Machtei EE. The effect of membrane exposure on the outcome of regenerative procedures in humans: a meta-analysis. J Periodontol (1970). 2001;72:512–516.
- Chaushu G, Mardinger O, Peleg M, Ghelfan O, Nissan J. Analysis of complications following augmentation with cancellous block allografts. J Periodontol (1970). 2010;81:1759–1764.
- Checchi V, Gasparro R, Pistilli R, Canullo L, Felice P. Clinical classification of bone augmentation procedure failures in the atrophic anterior maxillae: esthetic consequences and treatment options. BioMed Res Int. 2019;2019:4386709–4386716.
- Buser D, Dula K, Belser UC, Hirt HP, Berthold H. Localized ridge augmentation using guided bone regeneration. II. Surgical procedure in the mandible. Int J Periodontics Restorative Dent. 1995;15:10–29.
- Kfir E, Kfir V, Eliav E, Kaluski E. Minimally invasive guided bone regeneration. J Oral Implant. 2007;33:205–210.
- Mazzocco C, Buda S, De Paoli S. The tunnel technique: a different approach to block grafting procedures. Int J Periodontics Restorative Dent. 2008;28:45–53.
- De Stavola L, Tunkel J. Results of vertical bone augmentation with autogenous bone block grafts and the tunnel technique: a clinical prospective study of 10 consecutively treated patients. Int J Periodontics Restorative Dent. 2013;33:651–659.
- Xuan F, Lee C-U, Son J-S, Fang Y, Jeong S-M, Choi B-H. Vertical ridge augmentation using xenogenous bone blocks: a comparison between the flap and tunneling procedures. J Oral Maxillofac Surg. 2014;72:1660–1670.
- Restoy-Lozano A, Dominguez-Mompell JL, Infante-Cossio P, LaraChao J, Espin-Galvez F, Lopez-Pizarro V. Reconstruction of mandibular vertical defects for dental implants with autogenous bone block grafts using a tunnel approach: clinical study of 50 cases. Int J Oral Maxillofac Surg. 2015;
44:1416–1422. - Misch CE. Divisions of available bone in implant dentistry. Int J Oral Implantol. 1990;7:9.
- Liang W. Vascularized buccal inversion flap. J Oral Implantol. 2016; 42:421–425.
- De Stavola L, Tunkel J. Results of vertical bone augmentation with autogenous bone block grafts and the tunnel technique: a clinical prospective study of 10 consecutively treated patients. Int J Periodontics Restorative Dent. 2013;33:651–659.
- Restoy-Lozano A, Dominguez-Mompell JL, Infante-Cossio P, LaraChao J. Reconstruction of mandibular vertical defects for dental implants with autogenous bone block grafts using a tunnel approach: clinical study of 50 cases. Int J oral Maxillofac Surg. 2015;44:1416–1422.
- de Azevedo RA, Matos FS, Figueiredo LMG. Appositional bone graft tunneled: technical note. Int J Surg Case Rep. 2017;33:143–147.